Abstract
COVID-19 is the most significant public health emergency in more than a century, caused a global economic crisis, and has long-term repercussions across society. This unprecedented crisis has highlighted the urgent need for smart investments to strengthen health system resilience. There is a need to protect people’s underlying health; fortify the foundations of health systems; and bolster health professionals working on the frontline. This report identifies a set of priority investment areas needed to strengthen health system resilience. It then produces order-of-magnitude estimates of the expected costs of such investments, drawing extensively from existing OECD data and analytical studies. These priority investments represent an estimated 1.4% of GDP, on average across OECD countries (and ranging from 0.6-2.5%), as compared with pre-pandemic expenditure of 8.8%. A combination of targeted spending and measures to reduce wasteful spending could mitigate the overall increases in health spending in the medium to long term.
Summary
More than two and a half years into the pandemic, countries around the world continue to feel the impact. COVID‑19 has been the most significant public health emergency in more than a century, caused a global economic crisis, and with long-term repercussions across society. COVID‑19 continues to claim lives, many are suffering longer term effects (physical and/or mental) due to the virus, and health systems are struggling to recover from the massive disruption.
These adverse effects highlight the need for smart investments to strengthen health system resilience – to protect underlying population health, fortify the foundations of health systems, and bolster health workers on the frontline – providing countries with the agility to respond not only to evolving pandemics but also to other shocks, whether natural or man-made. The return from such investments extends far beyond direct health benefits. More resilient health systems are at the core of stronger, more resilient economies – enabling substantial economic and societal benefits by avoiding the need for stringent and costly containment measures in future crises with healthier and better prepared societies.
Drawing on existing OECD data and analytical studies, an order-of-magnitude estimate of the costs of such investments represents an estimated 1.4% of OECD’s average GDP (ranging from 0.6‑2.5% across OECD countries). The total cost of these investments is set in the context of the pre‑pandemic situation; that is, in relation to the level of health expenditure in 2019 – equating to around 9% of the total OECD spent on health in 2019, or USD 627 billion (USD 460 per capita). This figure is similar to public funding across the OECD for prescription drugs. One could point to the 0.9 percentage point jump in the health spending to GDP ratio in 2020 and 2021 as a significant move towards this target. But this increase in health spending in 2020 and 2021 relative to GDP was driven both by the significant fall in GDP and the rapid surge in additional funding to the health sector to respond to the crisis. Much of this additional expenditure was in the form of emergency funding to firefight the pandemic, rather than long-term planned investments to strengthen resilience.
Previous work by the OECD Health Division has highlighted the enormous potential to make savings by tackling wasteful spending and realise efficiency gains across the health sector. A combination of targeted spending and measures to reduce wasteful spending could mitigate the overall increases in health spending in the medium to long term.
Here, the concept of resilience underpinning this analysis embraces but goes beyond just preparedness. Resilience is understood as the ability of systems to anticipate, absorb, adapt, and recover from major shocks such as COVID‑19 (OECD, 2020[1]). Resilience is not simply about minimising risk and avoiding shocks but recognising that shocks will happen. Such shocks are defined as high consequence events that have a major disruptive effect on society. Along with COVID‑19, this includes other highly infectious pathogens or emerging diseases. But it also covers natural or human-caused disasters that can lead to massive surges in health care needs. The investment areas and indicative cost estimates are relevant for both combatting COVID‑19 and other major emerging shocks.
The key investments needed to strengthen health system resilience
Investments for strengthening health system resilience can be grouped into three overarching investment pillars (Figure 1). These pillars aim to:
Protect people’s underlying health
Fortify the foundations of health systems
Bolster health professionals working on the frontline
For each of the three pillars, the key investments are identified. These are based on emerging evidence of the most effective policies in combatting COVID‑19, combined with evidence from experiences with managing previous major health shocks (see the OECD Digital Hub on Tackling the Coronavirus, https://www.oecd.org/coronavirus). Such investments have the benefit of making health systems better positioned to combat gradual transitions, such as demographic change and the increasing burden of chronic illnesses.
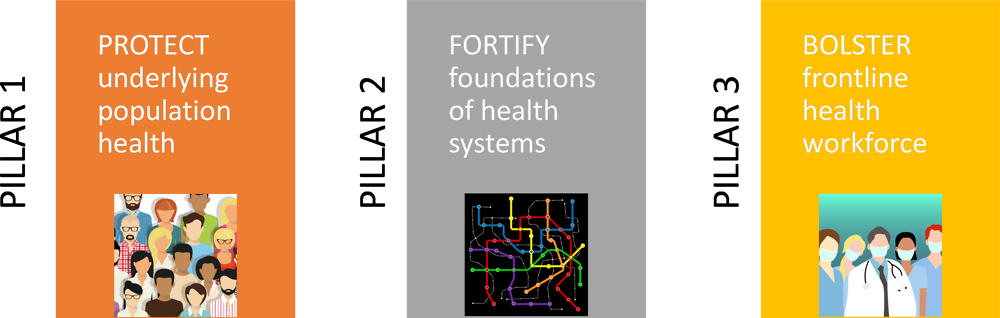
Image credit: Diagram uses images from © Shutterstock.com/Julia Tim; © Shutterstock.com/JMiks and © Shutterstock.com/SanXuan.
While investments require resources both up front and over time, they offer a substantial return – both in normal times, as well as during an ongoing pandemic or other emerging health shock. Here we focus on the costs of implementing priority investments into health systems. The amount of additional investment needed will vary by country, depending on existing capacities, with each country having areas where they will need to invest more, and areas where additional spending may not be needed. Indeed, into the third year of the pandemic, many countries have already started to make significant inroads into the investment gaps identified. Such variation is reflected in the range of estimates, notwithstanding that costing reflects broad order-of-magnitude estimates rather than any precise cost-accounting analysis.
Costing draws heavily on a rich body of information contained in OECD Health Statistics and recent OECD studies, supplemented by third-party sources providing more detailed epidemiological data and unit costs for some of the major inputs. The estimates – expressed as an additional share of GDP – give a sense of the scale of expenditure needed to strengthen health system resilience in OECD countries, whilst reflecting cross-country differences in these costs. For a more in-depth discussion of the methodological approach taken, see Morgan and James (2022[2]), from which this policy brief is based.
How much will investments to strengthen health system resilience cost?
Taken together, the seven key investments identified in this brief are estimated to be in the order of magnitude of about 1.4% of GDP (of which 0.13% is capital spending), on average across OECD countries, relative to pre‑pandemic spending of 8.8% of GDP. In other words, if all these investments had been made on top of existing health spending, the average OECD health spending to GDP ratio would have reached 10.1%, compared to the actual baseline average of 8.8% in 2019. The trajectory is based on an increase in the health spending-to-GDP ratio of this magnitude being reached at some point in the medium-term future (Figure 2). The total investment cost ranges from 0.6% to 2.5%, depending on how much a country is already spending on some of the investment areas.
Source: Secretariat calculations.
Bolstering health professionals working on the frontline accounts for more than half of this investment cost, on average, at around 0.7% of GDP (Pillar 3). Additional spending on preventive care is expected to cost about 0.3% on average (Pillar 1). Together, these can be seen as broadly consistent with recent analysis calling for countries to allocate an additional 1% of GDP for primary health care (WHO, 2019[3]) (WHO 2019). In addition, foundational investments in core equipment and the better harnessing of health information are estimated to cost about 0.4% of GDP on average (Pillar 2).

Source: OECD Secretariat calculations.
Pillar 1: Protect people’s underlying health
Investment 1: Enhanced preventive care
Preventive care is one of the cornerstones of an effective health system. In broad public health terms, whether interventions are targeted at individuals or populations, the aim is to enhance health status and maintain a state of low risk for diseases, disorders, or conditions. That is, effective preventive care policies limit the occurrence of new diseases and reduce the incidence of existing communicable and non-communicable diseases.
At a broad population level, experience from the COVID‑19 pandemic has shown that an effective public health surveillance system is an important policy lever to improve preparedness, particularly in monitoring and controlling the spread of an infectious disease (OECD, 2020[4]). This requires a well-functioning national and regional public health system with trained staff, an adequate availability of diagnostic laboratory equipment, and a capacity to rapidly ramp up the extent of testing and monitoring as future public health crises arise.
While a growing body of evidence shows that many health promotion and disease prevention measures can improve health outcomes at relatively low cost, health spending data shows that only around 2.7% of overall health spending is allocated to prevention activities (Gmeinder, Morgan and Mueller, 2017[5]). After taking into account a package of population health measures, a modest increase in the overall spending on prevention (to 0.3% of GDP) to match higher performing public health systems among OECD countries should see systems better resourced to meet future crises.
COVID‑19 has demonstrated the importance of strong infection prevention and control policies in health care settings. This includes health and long-term care workers adopting a number of common-sense precautions, notably: hand hygiene, environmental cleaning, and decontamination of medical equipment, aseptic techniques, and injection safety (WHO, 2021[6]). Of particular concern in recent years is an increasing degree of anti-microbial resistance (AMR). The OECD report ‘Stemming the Superbug Tide: Just A Few Dollars More’ showed that the burden of AMR on population health can be drastically reduced through cost-effective policies, such as the ending of over-prescription of antibiotics, rapid testing for patients to determine whether they have viral or bacterial infections, delays in prescribing antibiotics and promoting better hygiene (OECD, 2018[7]).
Investing more in health promotion and disease prevention also improves people’s underlying health. Despite clear progress in certain areas, such as preventive cancer screening programmes, policy levers to lower smoking and alcohol consumption and improve healthy diets, much more can still be done to reduce the major risk factors for health of alcohol, smoking, opioid use, and obesity. These risk factors not only increase the risk of non-communicable diseases, but also make people much more vulnerable to COVID‑19, other infectious diseases, and certain disasters.
To tackle harmful alcohol consumption, the 2021 OECD report Preventing Harmful Alcohol Use identified a package of the most effective interventions, including raising alcohol taxation, regulation of alcohol advertising, sobriety checkpoints to counter drink-driving and alcohol counselling in primary care (OECD, 2021[8]). Additional innovative policies include minimum unit pricing (MUP) and statutory bans on alcohol advertising targeting children.
For obesity the OECD report The Heavy Burden of Obesity listed food labelling, advertising restrictions and mass media campaigns as some of the key policies already implemented – to differing extents – in many OECD countries (OECD, 2019[9]). Additional policy measures that show promise encompass menu labelling, prescribing physical activity and workplace wellness programmes.
For other public health challenges such as tobacco and substance abuse, (OECD, 2019[10]), there has been less work to date in assessing the cross-country costs of a suitable package of measures. But a level of investment similar to the package of measures to tackle alcohol abuse might be assumed. Taken together, the range of public health interventions would amount to a modest increase of around USD 15 per capita.
Investment 2: Mass population programmes
In addition to a stronger public health system, countries will need to be prepared for mass population programmes that protect people’s underlying health and enable countries during acute phases of a health shock. For COVID‑19, most notable is the need to develop and maintain vaccination campaigns. This includes staffing and other associated delivery costs, as well as the costs of the vaccines themselves. Note that such estimates exclude the expected costs of R&D for new vaccines and treatments for COVID‑19 and other emerging pathogens. Testing has proved an important complementary policy prior to and in parallel with vaccination campaigns, particularly during the various stages of a pandemic.
Mass vaccination programmes have reduced the risk of serious illness from COVID‑19, and consequently hospitalisations. Most OECD member countries have aimed to administer two or three COVID‑19 vaccine doses to the vast majority of their population. Moving forward, there is considerable uncertainty regarding how frequently COVID‑19 vaccinations will be needed. Some researchers cite emerging evidence that three doses is sufficient to provide long-lasting protection from new as well as existing variants, while others emphasise long COVID‑19 and the need for annual vaccination campaigns against influenza at least for the more vulnerable groups of the population (Dolgin, 2021[11]; Muecksch et al., 2022[12]; Rubin, 2021[13]).
For vaccines, whilst the purchase cost of a vaccine against COVID‑19 particularly early on was variable, media reports1 reporting a range from as low as USD 3 to over USD 30 per dose. As with mass testing, these costs may fall over time. But costs do not include the associated costs of delivery. A comprehensive study investigating the total cost (including the cost of delivery) of vaccinating against 17 pathogens over a lifetime in seven western European countries gave a five‑fold cost range of EUR 44 to EUR 226 per pathogen (Ethgen et al., 2016[14]). Narrowing down these estimates to only vaccination costs for healthy individuals (as compared with vaccinations for people with health complications) gave a range of EUR 37 to EUR 132 per pathogen.
For testing, data collated from eight OECD countries of the cost of a PCR test, together with associated delivery and laboratory costs, point to an average per capita cost of around USD 80 (ranging from around USD 55‑100). Again, unit costs of testing tend to fall – for example, as the extended use of antigen tests for COVID‑19 provided an initial result without the need of a laboratory process. However, such potential cost reductions over time in both vaccines and testing are not accounted for in the final cost estimates.
To reach an estimate of the level of expenditure required to perform effective testing and vaccination on an annual basis, unit cost estimates are combined with the share of the population expected to need each of these interventions. A one‑to‑one relationship is assumed for simplicity between mass testing and vaccinations. That is, as vaccinations are gradually scaled up, testing is concurrently scaled down at the same rate.
Given the uncertainty around vaccine availability and effectiveness in reducing severity of disease, and the needed levels of diagnostic testing, a range of scenarios is examined. A low scenario assumes 40% of the population aged under 65 years are tested or vaccinated against COVID‑19 each year, with 80% coverage for the population aged 65 years and above. A high scenario assumes 80% coverage for people aged under 65 years, and 95% coverage for people aged over 65 years. The mid-point scenario assumes 60% coverage for people aged under 65 years, and 80% coverage for older populations. Combining this mid-point coverage with an assumed annual unit cost of USD 100 for diagnostic testing and/or vaccination, the additional spending required is equivalent to 0.15% of GDP on average, ranging from 0.05 to 0.35%.
COVID‑19 has also shown the importance of ensuring sufficient supplies of personal protective equipment (PPE) during acute phases of a health shock. All countries will need to have the capacity to ramp up PPE supplies and testing efforts for future COVID‑19 peaks, or indeed for other emerging infectious pathogens.
To maintain adequate stocks of PPE to manage acute phases of a health shock, estimates of additional spending needs are based on having sufficient supplies in hospitals, primary care, and long-term care facilities for a 100‑day wave of COVID‑19 (or other emerging pathogen with an equivalent degree of infectiousness). The quantities of specific PPE needed are based on an epidemiological model developed by Johns Hopkins University – of additional PPE needs over and above what is needed in normal times (Johns Hopkins University, 2020[15]). They calculate that, on a per capita basis, 10.28 gloves, 0.97 isolation gowns, 0.54 medical-grade masks and 0.17 N95 masks will be needed during a 100‑day wave (on average) with sustained suppression measures in place. Added in this report are needs for face shields and goggles. Multiplied by unit cost estimates from the World Health Organization (2020[16]) with a 10% price mark-up, this translates into an average cost of USD 10.75 per capita to provide sufficient PPE within different health and long-term care settings. The estimates do not consider the impact due to disruptions in supply chains due to, for example, geopolitical and trade tensions.
Pillar 2: Fortify the foundations of health systems
Investment 3: Sufficient core equipment
The COVID‑19 crisis has seen health care systems, and hospitals, placed under immense strain. Some countries have lacked sufficient physical resources, notably in terms of hospital beds and other medical equipment to respond to the sudden influx of COVID‑19 patients and their subsequent treatment (OECD, 2020[4]). Investing to provide a certain base level of core equipment needs is seen as a prerequisite to strengthening overall health system resilience and continuing to meet standards of care during a health shock. Having sufficient medical equipment in intensive care units and other settings helps avoid potentially catastrophic delays in diagnosing and treating patients, as well as minimising circumstances where there are more patients than beds. However, ensuring sufficient capacities are available in times of crisis may result in some redundancy in normal times.
Non-medical equipment is also important, notably computers and other IT equipment. An adequate physical IT infrastructure provides the basis for trained health professionals to better monitor patients’ health, both in acute situations and in the long term. Used correctly, telemedicine can make care more responsive, leading to increased quality and efficiency.
There are no hard and fast guidelines or international benchmarks regarding the optimal level of equipment and technology, with large variability across OECD countries. Indeed, some may be surplus to requirement, and needs to be weighed up against the opportunity cost of equipment not being sufficiently utilised during routine periods. Still, what is clear is the critical importance of maintaining some spare capacity to deal with surges – too little investment in medical equipment will lead to strains in service provision and preventive care efforts, thereby undermining health system resilience.
On average, OECD countries invest on average around 0.25% of GDP each year on transport, machinery, and equipment (both medical and non-medical) as well as IT hardware in the health and social sector. Based on the scenario that all OECD countries should reach the 75‑percentile level in terms of annual investment in equipment, this would result in an average increase as a share of GDP of 0.08%.
The same approach can determine the level of capital spending needed to maintain responsive health information systems, beyond the physical ICT hardware; that is, spending on the development of software and databases in the health and social sector. An increase in capital spending to bring the level up to the 75% percentile would equate to an average increase of 0.05%.
Investment 4: Well-harnessed health information
Beyond the capital investments, better use of health data produced is critical. This reflects ongoing deficiencies that exist in the health sector – a sector where correct decisions can have considerable impact but a sector that remains “data rich but information poor”. Improved IT linkages are needed to move information to where it is needed, not only within the health system but also externally; for example, facilitating whole of government decision making by balancing information on health system capacity versus containment and mitigation decisions.
Judicious use of routine health data improves containment and mitigation efforts, including early warning systems, and ensures patients receive the right care for their needs (including the wider adaptation of telemedicine) and are adequately followed up. To strengthen trust in digital health solutions, there is a need to ensure that the use of such personal data is responsible and well informed. This includes enabling privacy and ensuring personal data protection, digital security, and promoting the interoperability and governance of health data.
The OECD report Health in the 21st Century concluded that health lags behind many other parts of the economy in harnessing the potential of data and digital technology, “missing the potential to save a significant number of lives and billions of dollars” (OECD, 2019[17]). The report concluded that a conservative doubling of current investment levels is needed to promote more intelligent use of data for information and knowledge, and that this could equate to a healthy return of approximately 3 to 1.
Assuming that overall higher spending countries are already more advanced in harnessing their health data and information, an inversely proportional additional investment range of 2‑4% of health care expenditure is applied, in line with the OECD’s Health in the 21st Century report. Using health spending data across OECD countries in 2019, the level of additional investment would equate to 0.26% of GDP.
Pillar 3: Bolster health professionals working on the frontline
Investment 5: Sufficient health and long-term care professionals
At the heart of health system resilience is a stronger frontline. Concerns about the retention of staff, and associated labour and skill shortages, have been accumulating over the years. Increased pressure from demographic change, population demands and added concerns that the upcoming retirement of an older generation of doctors and nurses are expected to further exacerbate such shortages (OECD, 2016[18]).
Securing sufficient numbers of skilled health and care professionals – in hospitals, across primary care, and in long-term care – is essential. A reinforced workforce strengthens service delivery, enabling effective case management of individuals with COVID‑19 (or those hospitalised due to other types of health shocks), while also maintaining services at all levels of a health system for other health care needs.
The pandemic has heightened the awareness from governments and citizens alike that nursing and care staff deserve greater recognition for the skill, responsibility, and empathy they demonstrate on a daily basis. During the first and subsequent waves of the pandemic, health and care workers have been at the frontline, enduring long and difficult working conditions with increased risk of infection, serious illness, and death.
Costing the investment needs are broken down into two major cost drivers: (1) the cost of having an adequate number of health and long-term care professionals; and (2) the cost of improving the competitiveness of salaries of key cadres of health and long-term care workers.
Building an adequate health workforce
Notwithstanding the many factors determining the optimal density of medical professionals in any one country – demographic and disease patterns, geographical and rural/urban characteristics as well as the organisation of care across providers – a simple international benchmarking provides order-of magnitude cost estimates for increases in staffing required for countries with relatively low numbers of health professionals.
Various thresholds for determining health worker densities have been put forward. The 2006 World Health Report identified a minimum health worker density of 2.3 skilled health workers (physicians and nurses/midwives) per 1 000 population used in monitoring their progress towards meeting the Sustainable Development Goals (SDGs). The Global strategy on human resources for health: Workforce 2030 report considered an updated threshold of 4.45 health workers per 1 000 to reflect the broader range of services targeted by Universal Health Care (UHC) and the SDGs, while acknowledging that OECD health systems go beyond the provision of essential health services with a density of health workers above this threshold (WHO, 2016[19]). More pertinent in the analysis undertaken as part of the Global Burden of Disease Study 2019 to measure human resources for health in relation to universal health coverage, the Institute for Health Metrics and Evaluation (IHME) derived levels of health worker density (3.54 physicians and 11.45 nurses/midwives per 1 000 population) required to achieve a performance target of 90 out of 100 on the UHC effective coverage index (GBD 2019 Human Resources for Health Collaborators, 2022[20]).
Bringing the density of physicians up to this threshold (and assuming current remuneration levels of physicians) for all OECD countries would require an average investment of 0.15% of GDP. The increase in the number of nurses across OECD countries to reach the threshold would require a further investment of around 0.33% of GDP on average.
The number of personal care workers in the Long-term care (LTC) sector have also proved to be a key factor in mitigating the effects of the pandemic in the elderly population. Even some of the best-staffed high-income OECD countries do not rate the availability of LTC workers in their country as satisfactory (Colombo et al., 2011[21]). A study by the ILO on coverage deficits in long-term care sought to establish a minimum threshold for the provision of care based on the median population weighted value of selected OECD countries (ILO, 2015[22]). Meeting such a threshold, while recognising the very low levels in some countries, would equate to an average investment of 0.04% of GDP.
Taken together with physicians and nurses, this amounts to a net increase of more than three and a half million health and care professionals across all OECD countries.
Raising the competitiveness of salaries for nurses and care workers
Estimates of the costs of increasing salaries for nursing and personal care workers utilise OECD data on the current and additional number of health and care workers across various categories, along with reported levels of remuneration for 2019 available for hospital nurses in 35 OECD countries. This is combined with data on the relative salaries of different cadres of nurses and carers. The OECD publication ‘Who Cares?’ corroborates the UK and Swedish data, providing salary comparisons between carers and broader groups of nurses and health workers (OECD, 2020[23]).
Increasing the wages of nursing and care workers, using as a base the average OECD nurse salary level (relative to average national income) corresponds to an average increase of 0.14% of GDP.
Investment 6: Medical reserve
Boosting and optimising the capacity of health systems to respond to the surge in the demand for care associated with COVID‑19 cases has been one of the major challenges faced by countries, particularly early in the pandemic. As doctors, nurses and other health professionals were mobilised to play the role of first responders, health systems sought ways to rapidly increase the number of staff available. Several countries mobilised inactive and retired health professionals. Other countries turned to military health professionals, to assist in testing, treatment and in the relocation of patients. Countries have also mobilised students in medical, nursing, and other health education programmes to provide services to patients or to help in responding to public concerns, for example, staffing telephone hotlines or taking on the non-clinical tasks of key clinical staff.
Creating a medical reserve can offer a flexible and cost-effective surge capacity that can be called upon in times of high need. Costs relate primarily to recurrent training, to ensure people enlisted in a country’s medical reserve maintain the necessary skills to support full-time health professionals, and how they can integrate to best effect during a peak in COVID‑19 cases or other emerging health shock. Note that estimates do not include additional costs associated with the deployment of surge capacity during a health shock (e.g. per diems and travel allowances).
Based on the annual budgets for this type of entity, the annualised cost to develop and maintain a Medical Reserve Force are estimated to be in the range of 0.02 and 0.04% of GDP. This excludes additional costs associated with the deployment of surge capacity during a health shock (e.g. per diems and travel allowances).
Conclusions
Targeted investments in health systems strengthen resilience to both the ongoing pandemic and emerging future shocks. In doing so, they protect society and stimulate the economy. This brief has identified six key investments under three overarching pillars that aim to (1) protect people’s underlying health; (2) fortify the foundations of health systems; and (3) bolster health and long-term care professionals working on the frontline.
Taken together, the six investments amount to an estimated 1.4% of GDP on average, with a cross-country range of 0.6% to 2.5%, depending on how much a country is already spending on each of these investments. These estimates are based on such increases in the health spending to GDP ratio being reached and then spending in these areas maintained over time. Such numbers reflect broad order-of-magnitude estimates rather than results based on a precise cost-accounting analysis.
Funding such investments requires buy-in from ministries of finance as well as health ministries and social security institutions. Moving forward, the return from these targeted health system investments is likely to far outweigh the cost. For example, effective interventions in preventive care would eventually reduce the need for health care, with consequent cost-savings.
Within the health sector, such investments stop the health system from being overwhelmed. In the medium-term, they can also increase efficiency by reducing ineffective and wasteful spending. Beyond the health sector, such investments will boost the economy. A stronger, more resilient health system helps reduce the stringency of containment and mitigation measures in the future. It strengthens human capital both now, through a healthier and more productive workforce, and in the future, through less disrupted societies.
References
[21] Colombo, F. et al. (2011), Help Wanted?: Providing and Paying for Long-Term Care, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/9789264097759-en.
[11] Dolgin, E. (2021), “Omicron is supercharging the COVID vaccine booster debate”, Nature, https://doi.org/10.1038/d41586-021-03592-2.
[14] Ethgen, O. et al. (2016), “The cost of vaccination throughout life: A western European overview”, Human vaccines & immunotherapeutics, Vol. 12/8, pp. 2029-2037, https://doi.org/10.1080/21645515.2016.1154649.
[20] GBD 2019 Human Resources for Health Collaborators (2022), “Measuring the availability of human resources for health and its relationship to universal health coverage for 204 countries and territories from 1990 to 2019: a systematic analysis for the Global Burden of Disease Study 2019”, Lancet, Vol. 399/10341, pp. 2129-2154, https://doi.org/10.1016/S0140-6736(22)00532-3.
[5] Gmeinder, M., D. Morgan and M. Mueller (2017), “How much do OECD countries spend on prevention?”, OECD Health Working Papers, No. 101, OECD Publishing, Paris, https://doi.org/10.1787/f19e803c-en.
[22] ILO (2015), Long-term care protection for older persons: a review of coverage deficits in 46 countries, International Labor Organization, Geneva, https://www.ilo.org/secsoc/information-resources/publications-and-tools/Workingpapers/WCMS_407620/lang--en/index.htm.
[15] Johns Hopkins University (2020), “Assumptions”, https://www.centerforhealthsecurity.org/resources/COVID-19/PPE/PPE-assumptions.
[2] Morgan, D. and C. James (2022), “Investing in health systems to protect society and boost the economy: Priority investments and order-of-magnitude cost estimates”, OECD Health Working Papers, No. 144, OECD Publishing, Paris, https://doi.org/10.1787/d0aa9188-en.
[12] Muecksch, F. et al. (2022), “Increased Potency and Breadth of SARS-CoV-2 Neutralizing Antibodies After a Third mRNA Vaccine Dose”, bioRxiv (pre-print), https://doi.org/10.1101/2022.02.14.480394.
[8] OECD (2021), Preventing Harmful Alcohol Use, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/6e4b4ffb-en.
[1] OECD (2020), “A systemic resilience approach to dealing with Covid-19 and future shocks”, OECD Policy Responses to Coronavirus (COVID-19), OECD Publishing, Paris, https://doi.org/10.1787/36a5bdfb-en.
[4] OECD (2020), How resilient have European health systems been to the COVID-19 crisis?, OECD Publishing, Paris, https://doi.org/10.1787/85e4b6a1-en.
[23] OECD (2020), Who Cares? Attracting and Retaining Care Workers for the Elderly, OECD Publishing, Paris, https://doi.org/10.1787/92c0ef68.
[10] OECD (2019), Addressing Problematic Opioid Use in OECD Countries, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/a18286f0-en.
[17] OECD (2019), Health in the 21st Century: Putting Data to Work for Stronger Health Systems, https://doi.org/10.1787/e3b23f8e.
[9] OECD (2019), The Heavy Burden of Obesity: The Economics of Prevention, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/67450d67-en.
[7] OECD (2018), Stemming the Superbug Tide: Just A Few Dollars More, OECD Health Policy Studies, OECD Publishing, Paris, https://doi.org/10.1787/9789264307599-en.
[18] OECD (2016), Health Workforce Policies in OECD Countries: Right Jobs, Right Skills, Right Places, https://doi.org/10.1787/9789264239517.
[13] Rubin, R. (2021), “Vaccine Makers Plan for Annual Boosters, but It’s Not Clear They’ll Be Needed”, JAMA, Vol. 326/22, pp. 2247-2249, https://doi.org/10.1001/jama.2021.21291.
[6] WHO (2021), Infection prevention and control in primary care: a toolkit of resources, World Health Organization, Geneva, https://www.who.int/publications/i/item/9789240037304.
[16] WHO (2020), Emergency Global Supply Chain System (COVID-19) catalogue: Meeting report, World Health Organization, Geneva, https://www.who.int/publications/m/item/emergency-global-supply-chain-system-covid-19-catalogue.
[3] WHO (2019), The Universal Health Coverage Global Monitoring Report 2019, World Health Organization, Geneva, https://www.who.int/docs/default-source/documents/2019-uhc-report.pdf.
[19] WHO (2016), Global strategy on human resources for health: Workforce 2030, World Health Organization, Geneva, https://www.who.int/publications/i/item/9789241511131.
Contact
Francesca COLOMBO (✉ [email protected])
David MORGAN (✉ [email protected])
Chris JAMES (✉ [email protected])
Note
See, for instance: https://www.ft.com/content/80f20d71‑d7eb‑4386‑b0f2‑0b19e4aed94d.