Abstract
The COVID‑19 crisis has heightened the risk factors generally associated with poor mental health – financial insecurity, unemployment, fear – while protective factors – social connection, employment and educational engagement, access to physical exercise, daily routine, access to health services – fell dramatically. This has led to a significant and unprecedented worsening of population mental health. Across countries, the mental health of unemployed people and those experiencing financial insecurity was worse than that of the general population – a trend that pre‑dates the pandemic, but seems to have accelerated in some cases. OECD countries have responded with decisive efforts to scale‑up mental health services, and put into place measures to protect jobs and incomes, thereby reducing mental distress for some. However, the scale of mental distress since the start of the pandemic requires more integrated, whole‑of-society mental health support if it is not to lead to permanent scarring.
Population mental health worsened markedly during the pandemic:
From March 2020 onwards, prevalence of anxiety and depression increased and in some countries even doubled. Periods when the highest rates of mental distress were reported correlated with periods of intensifying COVID‑19 deaths and strict confinement measures;
Across countries, the mental health of unemployed people and those experiencing financial insecurity was worse than that of the general population – a trend that pre‑dates the pandemic, but seems to have accelerated in some cases.
Mental health services were already over-stretched before 2020. The scale of mental distress since the start of the pandemic requires unprecedented levels of mental health support if it is not to lead to permanent scarring. OECD countries have taken immediate steps to increase mental health support:
Most countries developed new mental health information and/or phone support lines giving tips on coping measures during the COVID‑19 crisis, while many countries also increased entitlement to mental health services, and/or mental health funding;
Many OECD countries swiftly put in place measures to protect jobs and incomes, and aid the transition to working from home. Job retention schemes helped to support both the incomes and the mental health of workers;
Mental health support was weakly integrated in social welfare, labour and youth policies before the crisis. Beyond emergency measures, there is an urgent need to deliver stronger, more integrated policies to support mental health. An integrated whole‑of-society response means:
Access to existing mental health services should be assured either in-person or via telemedicine, or both, and increasing access to evidence‑based services should be a priority, including alternatives to mental health promotion programmes in schools or workplaces which have been particularly disrupted;
Employers must contribute to supporting the mental health of employees, including those who have been on job retention schemes. Policy makers should look further at the implications of long-term teleworking on mental health, and countries should consider scaling-up mental health support for jobseekers through public employment services.
The terms “mental health conditions” and “mental health issues” are used in this brief, while the terms “mental illness” and “mental disorder” are largely avoided. This is to align language with ongoing shifts that go hand-in-hand with efforts to raise awareness and address stigma, and to ensure, where possible, language is person-centred, strengths-based, and recovery-focused, and reflects the differing experiences of mental health issues from individual to individual.
Data on population mental health, and especially age‑stratified data, remains limited in coverage. This brief primarily uses prevalence symptoms of anxiety and depression, estimated through surveys, as a proxy for mental health. Where possible, surveys using validated instruments – such as General Anxiety Disorder (GAD‑7) for anxiety and Patient Health Questionnaire‑9 (PHQ‑9) for depression – are used. Samples are not necessarily representative, especially for those rapid surveys undertaken during the COVID‑19 crisis, and survey methods differ between studies, limiting the possibility for cross-country comparisons. As symptoms are self-reported, increase in prevalence may partially reflect changes in awareness or levels of stigma against individuals experiencing mental health issues, which can influence different national trends and trends across time.
Population mental health has deteriorated significantly since the start of the COVID‑19 pandemic
For decades, the prevalence of mental health conditions has been broadly unchanged; this trend changed in 2020 with the outbreak of the COVID‑19 pandemic. From March 2020 onwards, the prevalence of anxiety and depression increased. For example, in Belgium, France, Italy, Mexico, New Zealand, the United Kingdom and the United States, prevalence of anxiety in early 2020 was double or more than double the level observed in previous years; in Australia, Belgium, Canada, France, the Czech Republic, Mexico, Sweden, the United Kingdom and the United States, prevalence of depression in early 2020 was also double or more than double that observed in previous years.
During 2020, the risk factors for poor mental health – financial insecurity, unemployment, fear – increased, while protective factors – social connection, employment and educational engagement, access to physical exercise, daily routine, access to health services – decreased.
When compared to the results prior to the pandemic, the data consistently shows that rates of anxiety and depression increased in 2020 compared to previous years (Figures 1 and 2). Across OECD countries, different survey instruments have been used to measure the prevalence of anxiety and depression, and the levels of mental distress. The prevalence rates and the changes in these rates are not directly comparable across countries, and some surveys undertaken during 2020 do not cover nationally representative samples. Nonetheless, the prevalence of anxiety and depression has clearly increased significantly.
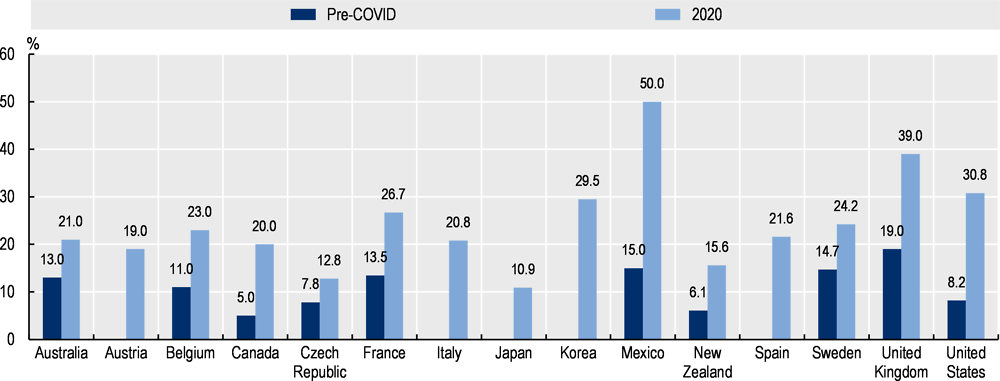
Note: ¹To the extent possible, 2020 prevalence estimates were taken from March-April 2020.
The survey instruments used to measure anxiety and population samples differ between countries, and therefore are not directly comparable, and some surveys may have small sample sizes and/or not use nationally representative samples. Differences in the openness of populations to discussing their mental state also hampers cross-country comparability. Where possible, surveys using the GAD‑7 instrument have been selected. 2013 data for Sweden uses a cut-off of ‘8’ for the GAD‑7, while most other studies use a cut off of ≥10.
Source: National sources: Australia 2017-18 and 2020; Austria 2020; Belgium 2018 and 2020; Canada ‘before COVID’ and 2020; Czech Republic 2017 and 2020; France 2017 and 2020; Italy 2020; Japan 2020; Korea 2020; Mexico 2019-20 and 2020; New Zealand 2016-17 and 2020; Spain 2020; Sweden 2013 and 2020; the United Kingdom 2019 and 2020; the United States 2019 and 2020.
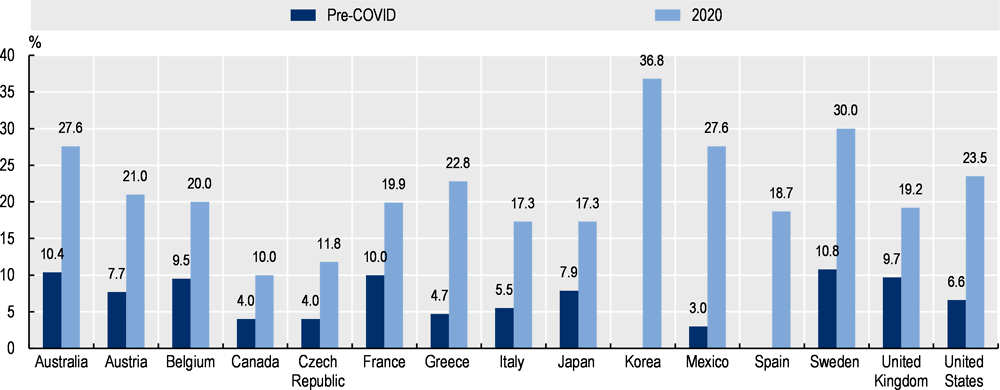
Note: ¹To the extent possible, 2020 prevalence estimates were taken from March-April 2020.
The survey instruments used to measure depression differ between countries, and therefore are not directly comparable, and some surveys may have small sample sizes or not use nationally representative samples. Differences in the openness of populations to discussing their mental state also hampers cross-country comparability. Where possible, surveys using the PHQ‑9 instrument have been selected. 2020 data for Sweden uses a cut-off of ‘11’ for the PHQ‑9, while most other studies use a cut off of ≥10.
Source: National sources Australia 2017-18 and 2020; Austria 2014 and 2020; Belgium 2018 and 2020; Canada ‘before COVID’ and 2020; Czech Republic 2017 and 2020; France 2017 and 2020; Greece 2014 and 2020; Italy 2014 and 2020; Japan 2013 and 2020; Korea 2020; Mexico 2019-20 and 2020; Spain 2020; Sweden 2013 and 2020; the United Kingdom 2019 and 2020; the United States 2019 and 2020.
A survey by the Commonwealth Fund conducted in the period March-May 2020 found that many adults reported experiencing stress, anxiety, or sadness that was difficult to cope with alone since the outbreak started. A high percentage of adults experienced this mental distress in Australia (23%), Canada (26%), France (24%), New Zealand (23%), the United Kingdom (26%) and the United States (33%), and lower rates of distress were seen in the Netherlands (14%), Norway (10%) and Sweden (18%) (Commonwealth Fund, 2020[1]). Other measures of population mental distress, including self-reported mental health status, distress, or sleep disturbance, confirm this trend of worsened population mental health status.
Population mental distress was highest during periods of intensifying COVID‑19 deaths and measures to limit transmission of the virus
Across 2020, and into 2021, the COVID‑19 crisis has seen different ‘waves’ of COVID‑19 cases, hospitalisations, deaths, and restrictions and measures to limit transmission. Population mental health has also gone up and down in different ‘waves’, with peaks of mental distress closely correlated with peaks in COVID‑19 deaths, and periods when pandemic control measures were most stringent. Mental distress was particularly high at the beginning of the crisis in March-April 2020, before improving somewhat towards the European summer, which coincided with falling COVID‑19 cases and relaxing of ‘lockdown’.
In countries which regularly measure levels of mental distress among the general population during the course of 2020 – Canada, France, New Zealand, the Netherlands, the United Kingdom, the United States – anxiety and/or depression levels were highest between mid-March and early April 2020, before falling around June‑July 2020, and then rising again from September 2020 onwards. Generally, countries saw very similar trends in mental well-being, which showed a fair degree of correlation with both the stringency of policies to contain the pandemic measured based on Oxford University/Blavatnik Stringency and Policy Index, and the number of deaths from COVID‑19 (measured using ‘excess deaths’), as seen in the examples from France, the Netherlands, and the United Kingdom (Figure 3).
The timeliness of survey efforts during the COVID‑19 crisis has also generated close to ‘real time’ insights into population mental health, a valuable source of information unseen in previous crises such as the 2008 financial crisis. It will be important to continue tracking mental health impacts as the crisis remains and even as the immediate health crisis subsides, to understand whether population burden of mental health conditions returns to the pre‑pandemic norm (an all-condition prevalence rate of around 20% of the working-age population (OECD, 2012[2]), or whether this higher prevalence rate for some conditions is the ‘new normal’. The policy implications of the latter would be significant.
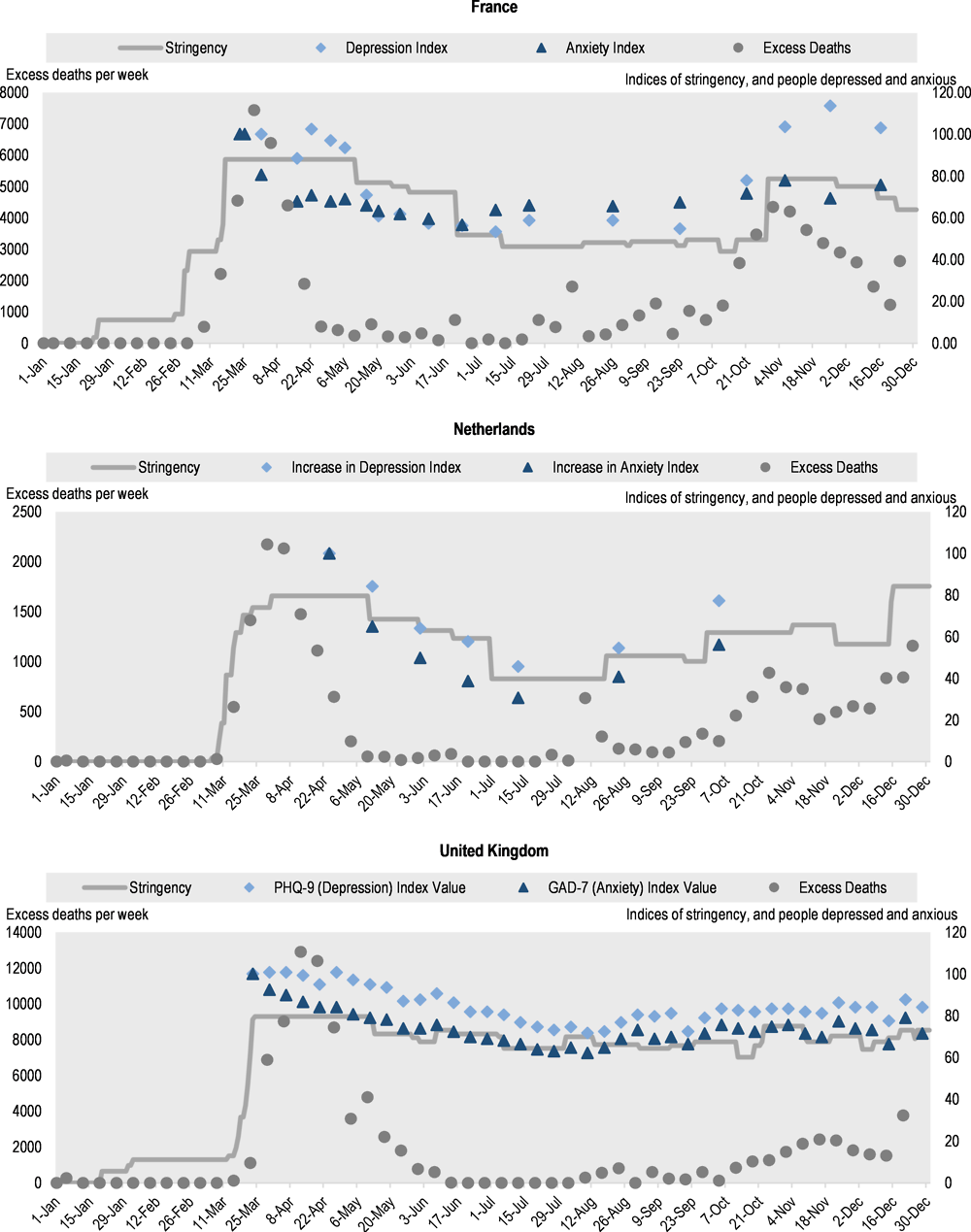
Note: ‘Stringency Score’ is based on Oxford University/Blavatnik Stringency and Policy Index. The stringency tracker comes from the Blavatnik School of Government, which calculates a stringency value using school closing, workplace closing, cancel public events, restrictions on gathering size, close public transport, stay at home requirements, restrictions on internal and international movement, and public information campaigns in each country. In each country, the first point of mental health data collected was assigned 100, and each subsequent data piece was defined in relation to the first data point in order to produce a comparable figure that tracked relative percentage change in data. Excess deaths are based on OECD data – COVID‑19 Health Indicators – Excess deaths by week. The survey instruments and population sampling approaches differ between countries, and are not directly comparable, and some surveys may have small sample sizes and/or not use nationally representative samples.
Source: Oxford University/Blavatnik Stringency and Policy Index; OECD COVID-19 Health Indicators - Excess deaths by week; mental distress indices from France, Netherlands, UnitedKingdom.
People with less secure employment, lower educational status, and lower income are experiencing higher rates of mental distress during the COVID‑19 crisis
Risk of, and resilience to, poor mental health varies across population groups, and notably by age, gender, employment status, financial situation, and socio‑economic status. Young people, those living alone, those with lower socio-economic status, and those who were unemployed had higher rates of mental distress. Conversely, people who were able to continue working during confinement, including those who worked remotely, were less likely to report depression and anxiety, at least during the earlier stages of the crisis.
Being out of work during 2020 increased mental health risks. Longitudinal evidence from France (Figure 4) shows that individuals in employment have been less likely to report symptoms of depression and anxiety than unemployed people. Across the OECD, job retention or short-time work schemes were introduced or adapted to protect jobs, as these scheme allow employees to keep their contracts with the employer even if their work is suspended (OECD, 2021[3]). The French longitudinal data suggest that such schemes have cushioned the mental health impacts of the crisis. Similarly, in the United Kingdom, furloughed workers in long-term insecure jobs from before and during the pandemic reported no increase in mental distress, whereas workers who were not furloughed reported significant increase in mental distress (Smith, Taylor and Kolbas, 2020[4]).
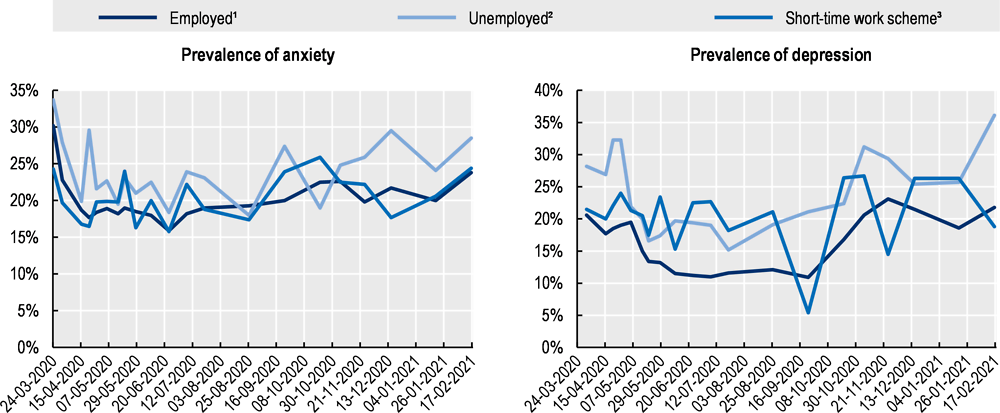
Note: ¹’Travail’ ²’Chomage’ ³’Chomage partiel’. Results are based on a survey with a small sample size (2 000 total respondents by survey wave) which may drive sharp drops and falls in some survey waves.
Source: Santé Publique France, Enquête CoviPrev, https://www.santepubliquefrance.fr/etudes-et-enquetes/coviprev-une-enquete-pour-suivre-l-evolution-des-comportements-et-de-la-sante-mentale-pendant-l-epidemie-de-covid-19.
Lower socio-economic status (SES) has long been associated with an increased risk of poor mental health (OECD, 2015[5]). This has continued during the COVID‑19 pandemic, with disadvantaged groups experiencing higher rates of mental distress. In the United Kingdom, an anxiety score was measured continuously for 20 weeks from the onset of the first lockdown in March 2020; higher anxiety scores were consistently reported amongst people with lower education or lower income (Fancourt, Steptoe and Bu, 2020[6]). Another report from the United Kingdom found that people whose income dropped and who became dependent from different forms of state support – such as universal credit or self-employment grants – or people experiencing long-term financial difficulties, experienced greater declines in their mental health than the population average during the first lockdown in April 2020 (NatCen Social Research, 2021[7]). However, trends in changing mental health status and SES are not consistent across all populations, and it has been hard to assess whether the mental health of people of lower SES has worsened faster or more compared to population averages. For example, in the United States, a survey in April 2020 actually found persons with higher SES (educational attainment and household income) reported sharper declines in life satisfaction and bigger increases in depressive symptoms than people with lower SES compared to survey results in 2019.
The prevalence of mental health conditions is also known to differ between men and women, with women more likely to report depression or anxiety. During the COVID‑19 crisis, the existing gender differences in the prevalence of anxiety and depression have widened. Evidence from the first wave of the COVID‑19 pandemic in the United Kingdom found that mental health deteriorated more among working parents compared to those without children, with working women reporting greater declines. In the United States, the gender gap in mental health widened by 66% in the initial stages of the pandemic between March and April 2020 (Adams-Prassl et al., 2020[8]).
Delivering an integrated whole‑of-society policy response to support mental health during and after the COVID‑19 crisis
To respond effectively to the impact of the COVID‑19 crisis on population mental health, integrated and cross-sectoral policies to improve mental health support are needed. Such efforts are called for in the OECD Recommendation on Integrated Mental Health, Skills and Work Policy, to which all OECD countries are adherents since 2015. The Recommendation, a result of the OECD’s long-standing work on mental health and work, suggests that through early intervention in youth, workplace and welfare policies, the social, educational and labour market outcomes of individuals experiencing mental health issues can be improved. Such approach built on early recognition and integrated services is ever more important now. Combined with broader strategies and campaigns, policies can reduce the stigma that surrounds mental health, and promote schools and workplaces that contribute to better mental health for the general population.
Safeguarding access to mental health services, and responding to the increased need for mental health care
During the COVID‑19 crisis, there have been significant disruptions to the delivery of mental health services. A WHO survey in the second quarter of 2020 found that more than 60% of countries worldwide reported disruptions in mental health services: 67% saw disruptions to counselling and psychotherapy; 65% to critical harm reduction services; and 35% reported disruptions to emergency interventions (WHO, 2020[9]). Similar trends are seen across mental health services in OECD countries. In Italy, in early April 2020, 14% of community mental health centres had been closed, 25% had reduced their hours, and approximately 78% of day hospitals had been closed, approximately 75% of non-urgent contacts were conducted remotely, primarily by phone (Carpiniello et al., 2020[10]). In the Netherlands, during the first wave of the pandemic, the number of referrals to mental health care fell by 25‑80%, demand for treatment dropped by 10 to 40%; billable hours decreased by 5‑20%; and bed occupancy dropped by 9% (GGZ Netherland, 2020[11]).
Mental health services quickly shifted to new modes of delivery, in particular the use of digital mental health care. In mid‑2020, more than 80% of high-income countries reported to the WHO that they had used telemedicine and online therapy to replace in-person mental health consultations, or the use of helplines. For example, the United States made changes around telehealth with federal regulations temporarily permitting unprecedented access across state lines and non-secure platforms. For instance, by the end of 2020, Kaiser Permanente, the largest managed care organisation in the United States with 12 million plan members, was delivering 90% of its psychiatric care virtually (Gratzer et al., 2020[12]; Torous and Keshavan, 2020[13]). The Centre for Addition and Mental Health (CAMH), the largest psychiatric teaching hospital in Canada, increased virtual care visits by 750%, from approximately 350 to 3 000 online consultations from March to April 2020 (Cisco Canada, 2020[14]).
Preliminary results have shown that clinicians and clients have been positive about the uptake of digital services for the delivery of mental health during the COVID‑19 crisis. Service users report both high levels of satisfaction with video-delivered services and good levels of adherence to treatment, and some practitioners report more frequent check-ins with clients.
In Australia, the crisis rapidly accelerated the use of telemedicine, and as of end-April 2020, half of all mental health services under the Medicare Benefits Schedule were provided remotely; by the end of 2020, when in-person service delivery resumed, the rate of telehealth services was still nearly 100 000 per week, compared to zero in March 2020 (Australian Institute of Health and Welfare, 2020[15]). In England (United Kingdom), mental health services moved significantly to non-face‑to-face formats (phone and video) in 2020; and all mental health services had lower rates of face‑to-face service delivery in April 2020 than the 2019 rate.
Other digital mental health tools are also being accessed more. In the United States, the online therapy company Talkspace saw a 65% increase in clients between mid-February and end-April, and a federal hotline for people in emotional distress experienced a 1 000% increase in calls in April 2020 compared to April 2019, and use of self-screening questionnaires on the website of the non-profit Mental Health America increased by 60‑70% over the course of the outbreak (National Council for Behavioral Health, 2020[16]; Mental Health America, 2020[17]). The COVID‑19 outbreak has also pushed governments to make online or digital mental health resources available. In mid-April 2020, the Canadian Government launched a new portal for mental health resources, Wellness Together Canada, which offers no-cost wellness self-assessment, tracking and support resources, and counselling by text or phone; Canada also allocated surge funding to the Canada Suicide Prevention Service and the Kids Help Phone distress lines, as well as including self-care advice in the Canada COVID‑19 app used to record potential COVID‑19 symptoms.
OECD countries must now increase availability of mental health services, and respond to increasing demand for care
Countries have responded to rising mental health needs, but mental health services were already struggling to meet demand. In some countries, the COVID‑19 crisis has increased unmet need for mental health care. In August 2020, 9.2% of surveyed adults in the United States reported that they needed counselling or therapy but did not get it in the four previous weeks, while in 2019, 4.3% of adults reported that over the past year they could not receive counselling or therapy due to cost in the past 12 months (Centers for Disease Control and Prevention, 2020[18]).
Most OECD countries have taken at least some steps to increase mental health support. In particular, countries have introduced new forms of mental health support including informational materials (mostly online), new mental health support phone lines, shifting mental health services to telemedicine formats and in some cases increasing service capacity or entitlement, and in some countries increasing investment in mental health. In Portugal, a free phone line with 24 hour psychological support from 63 mental health specialists (psychologists) has been created in partnership with the Ministry of Health, the philanthropic foundation Fundação Calouste Gulbenkian (donating EUR 300 million) and the charter of psychologists Ordem dos Psicólogos Portugueses.
Many countries were also able to shift at least some mental health services to phone or online formats, in some cases adding new services or entitlement to services. In Australia, entitlement to reimbursed psychological therapies under the Medicare Benefits Scheme was doubled, from 10 sessions to 20 sessions, and the Australian Government has provided extra funding to expand telehealth services for all Australians to enable health care access through tele or video consultations from home. In France, in response to concerns about the mental health status of university students during the COVID‑19 crisis and closure of universities, a ‘Chèque psy étudiant’ was introduced in February 2021 giving students three consultations with a psychologist or psychiatrist with no out-of-pocket costs.
A few countries have committed to new funding for mental health care in light of the toll the COVID‑19 crisis is taking on mental health. In Australia, the government announced AUD 5.7 billion funding for mental health and aged care under the country’s COVID‑19 pandemic plan; in Canada, the government invested CAD 11.5 million on projects to support the mental health of particularly vulnerable Canadians during the COVID‑19 crisis; in Ireland, additional funding was provided under the 2021 budget (EUR 38 million) for new mental health services in response to the crisis, along with an additional EUR 12 million for existing needs, a EUR 50 million total increase compared to the 2020 budget; the Latvia Government has diverted an additional EUR 7.12 million to mental health services in 2021 in response to the COVID‑19 crisis, including funding for mental health specialists, for family doctors providing mental health support, and for psycho‑emotional support for medical staff; and in February 2021, Chile announced that the budget for mental health would increase by 310% compared to the previous budget.
Adapting workplace policies to promote mental health amidst the COVID‑19 crisis and beyond
Since the onset of the COVID‑19 pandemic, millions of workers have experienced job loss, and most have seen significant disruptions to how their work is organised and experienced. Many workers are also still on job retention schemes, and may not have been at work for a whole year. Some workers such as those in essential services have had to continue to work in-person, in some cases facing increased risk of exposure to COVID‑19 infection and in all cases needing to take new steps to protect their health at work, while other workers suddenly shifted to telework often full-time and across many months.
Teleworking poses new challenges for the relationship between work and mental health, and all employers could do more to support workers’ mental health
The COVID‑19 crisis saw a massive increase in telework. Across the OECD, at the start of the pandemic, around 39% of workers suddenly shifted to telework. Existing literature from before the COVID‑19 crisis on the impact of telework on the mental health of workers is limited, and the findings are inconclusive (Oakman et al., 2020[19]). While there can be benefits associated with teleworking such as more flexible working arrangements, telework can also blur the boundaries between work and home, contribute to extended working hours, and result in a sense of detachment from the workplace, all of which can have a negative impact on mental health.
Prior to the crisis, it was widely acknowledged that remote workers spent more hours working than workers in offices across most OECD countries (Eurofound and International Labour Office, 2017[20]), a pattern also systematically seen during the COVID‑19 crisis. Remote workers are also working less regular hours. For instance, an Ipsos survey conducted in November to December 2020, and covering workers from 28 countries, of which 20 OECD countries, found that almost half the respondents (44%) indicated that they worked unconventional hours either ‘to a large extent’ or ‘to some extent’ as a result of the COVID‑19 pandemic (Ipsos, 2020[21]). Video meetings may also be more mentally taxing than in-person meetings and contribute to increased fatigue, and the blurring of boundaries between work and personal lives can contribute to reduction in sleep quality.
Telework can increase the risks of working long hours and burnout – managing the balance of work and life has been particularly hard for working parents juggling professional responsibilities along with increased childcare and home schooling burden.
Increased teleworking is also likely to last. In July 2020, 78% of employees in a survey in the EU‑27 reported wanting to continue working from home at least occasionally, even without COVID‑19 restrictions (Eurofound, 2020[22]). A survey in Japan found that 79% of employees wish to telework or occasionally telework beyond the COVID crisis (Persol Research Institute, 2020[23]). New working patterns demand new protections for workers’ mental health. In December 2020, prompted by challenges in maintaining work-life balance posed by telework, lawmakers in the European Parliament called for a law to give workers the right to digitally disconnect outside working hours without repercussion, following in the footsteps of France, Italy, Spain and Luxembourg which already had “right to disconnect” legislation in place.
Given the increased risks to the mental health of employees amidst the COVID‑19 crisis, employers can take proactive steps to provide and strengthen mental health support available to employees including for both in-person and remote employees. Many employees still feel that their employers are not taking sufficient measures to address the mental health issues arising from the pandemic. In a recent PwC survey of remote workers in the United States, for example, employees were 26 percentage points less likely than executives to say their companies were successful or very successful in supporting the mental health of workers (PwC, 2021[24]). While large employers in the United States are reporting expanding access to virtual mental health services for their employees amidst the pandemic, small and medium size employers may face greater challenges in making mental health support available.
Whole‑of-workplace initiatives can also help ensure work contributes to better mental health. The National Standard for Psychological Health and Safety in the Workplace, developed in 2013 by the National Mental Health Commission of Canada, offers a set of voluntary guidelines to support companies in developing workplaces that promote mentally healthy working environments. A key component is mental health training for line managers and executives, and thus governments should consider investing in awareness-raising campaigns and seek to promote implementation of mental health training for line managers and executives. A Deloitte survey in the United Kingdom in 2017 found that while around half of line managers believed basic training in mental health would be useful, less than a quarter reported actually receiving training. Effective management by line managers can contribute to a workplace culture that is conducive to open discussion of mental health, help prevent workplace conflicts that are major risk factors for poor mental health, and promote earlier identification of potential mental health issues.
Design job retention schemes to promote the mental health of workers
The COVID‑19 crisis has also profoundly impacted the employment landscape with the large‑scale use of job retention schemes. In the early stages of the crisis, countries acted swiftly to put in place or modify these schemes, and in this process, supported over 60 million jobs across the OECD, accounting for around 20% of dependent employment. Job retention schemes have also indirectly, at least initially, contributed to protecting beneficiaries from a deterioration in their mental health. What is less known, is the consequences of prolonged furlough or short-time work as some workers have now been on such schemes since the onset of the pandemic.
An analysis of the United Kingdom and EU countries finds that even with only eight hours of work per week, employees can gain most of the mental health benefits that come with employment (Kamerāde et al., 2019[25]). One way in which governments can thus contribute to supporting the mental health of individuals on job retention schemes is to encourage employers in sectors in which this is possible to reduce hours worked, rather than cutting them to zero, and consider amending existing job retention schemes to promote work-sharing and allow partial return to work. Twenty-three OECD countries had pre‑existing short-time work schemes, including Kurzabeit in Germany and the Employment Adjustment Subsidy in Japan, with many increasing the coverage and generosity of these schemes at the onset of the crisis. By contrast, when first announced, all new job retention schemes in the OECD, with the exception of Iceland’s, could only be used for employees whose work was cut to zero hours (OECD, 2020[26]). In both Denmark and the United Kingdom, schemes were later amended to make compensation available even for reduced hours.
Addressing poor mental health through strengthening public employment services
Losing a job and becoming unemployed can be a contributing factor to poor mental health. Across the OECD, around 10 million more people are unemployed than prior to the crisis, with job losses concentrated in most affected sectors such as leisure, hospitality, transportation and retail (OECD, 2021[27]). This challenge will also extend beyond the short term, as unemployment will likely remain above pre‑crisis levels through to 2022.
Supporting jobseekers back into employment through job-search support, counselling and training opportunities remains a key lever to promote better mental health among the working population. Preventing long-term unemployment should be a priority, as the longer joblessness lasts, the more detached jobseekers become from the labour market. This is a particularly serious challenge for young people and new graduates (OECD, 2021[3]). The mistakes of the global financial crisis must not be repeated, when the increase in unemployment far outpaced the rise in spending on active labour market policies, resulting in a 21% decrease in time spent with each client (OECD, 2011[28]). Countries may be looking to scale back elements of their employment services to ensure they have the capacity to meet increased demand amidst the COVID‑19 crisis. Yet one area where services should not be temporarily reduced or suspended is in mental health support. Even prior to the crisis, public employment services offered little access to support for individuals experiencing mental health conditions.
Given the increased prevalence of mental health issues, and the continuing difficult employment prospects, far from suspending integrated mental health and employment support, countries should consider scaling them up.
Measures also need to combine mental health support with employment support. Evidence shows that mental health treatment alone does not improve employment outcomes for individuals with mental health conditions, whereas integrated employment and mental health support has been shown to be effective in improving employment prospects (OECD, 2015[5]). Large‑scale implementation of integrated mental health and employment support still remains lacking in most OECD countries, with most efforts targeted at individuals experiencing severe mental health conditions.
Active labour market programmes themselves can also help to cushion the impact of damaging effects of unemployment on mental health. A study in the United Kingdom found that participants in these programmes are likely to self-report better mental health outcomes than other unemployed individuals, although still likely to report poorer mental health than those in work. Participation in active labour market programmes shares some aspects of employment such as providing routine and structure to daily life, offering opportunities to meet new people and socialise, and supporting the development and maintenance of social networks. While supporting jobseekers back to work should remain the focus of active labour market policies, there is thus also scope to consider the mental health implications when assessing the effectiveness and success of such policies.
Youth support systems, too, will play a vital role in supporting the mental health of future generations, as discussed in the OECD Brief on Mental Health, COVID‑19 and Youth (OECD, 2021[3])
Acknowledgements
This policy brief was prepared by Emily Hewlett, Shunta Takino, Yuka Nishina and Christopher Prinz. Valuable comments were provided by colleagues across the OECD, in particular Stefano Scarpetta, Mark Pearson, Francesca Colombo, Masato Hayashikawa, Lara Fleischer, Jessica Mahoney, Muriel Levy and Nikita Arora.
For more details on the data sources and the measurement methodology, as well as further policy analysis of countries’ responses to the mental health impact of the COVID‑19 crisis, please see the forthcoming OECD Working Paper on ‘Tackling the mental health impact of the COVID‑19 crisis through an integrated whole‑of-society response’.
References
[8] Adams-Prassl, A. et al. (2020), “The Impact of the Coronavirus Lockdown on Mental Health: Evidence from the US”, Cambridge Working Papers in Economics, Faculty of Economics, University of Cambridge, https://www.repository.cam.ac.uk/handle/1810/310906 (accessed on 22 March 2021).
[15] Australian Institute of Health and Welfare (2020), Mental health services in Australia - Mental health impact of COVID-19, https://www.aihw.gov.au/reports/mental-health-services/mental-health-services-in-australia/report-contents/mental-health-impact-of-covid-19 (accessed on 11 February 2021).
[10] Carpiniello, B. et al. (2020), “Mental health services in Italy during the COVID‐19 pandemic”, Psychiatry and Clinical Neurosciences, Vol. 74/8, pp. 442-443, http://dx.doi.org/10.1111/pcn.13082.
[18] Centers for Disease Control and Prevention (2020), Mental Health - Household Pulse Survey - COVID-19, https://www.cdc.gov/nchs/covid19/pulse/mental-health.htm (accessed on 30 November 2020).
[14] Cisco Canada (2020), CAMH enhances virtual capacity to respond to demand for mental health services, https://newsroom.cisco.com/press-release-content?articleId=2072576 (accessed on 22 February 2021).
[1] Commonwealth Fund (2020), Do Americans Face Greater Mental Health and Economic Consequences from COVID-19? Comparing the U.S. with Other High-Income Countries | Commonwealth Fund, https://www.commonwealthfund.org/publications/issue-briefs/2020/aug/americans-mental-health-and-economic-consequences-COVID19 (accessed on 3 December 2020).
[22] Eurofound (2020), Working during COVID-19, https://www.eurofound.europa.eu/data/covid-19/working-teleworking (accessed on 17 February 2021).
[20] Eurofound and International Labour Office (2017), Working anytime, anywhere : the effects on the world of work., http://eurofound.link/ef1658 (accessed on 17 February 2021).
[6] Fancourt, D., A. Steptoe and F. Bu (2020), “Articles Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study”, The Lancet Psychiatry, http://dx.doi.org/10.1016/S2215-0366(20)30482-X.
[11] GGZ Netherland (2020), Parliamentary Consultation on Cornonavirus - GZZ Netherlands[Internetconsultatie gevolgen coronamaatregelen], https://www.tweedekamer.nl/sites/default/files/atoms/files/reader_internetconsultatie_coronamaatregelen.pdf1j0j7&sourceid=chrome&ie=UTF-8 (accessed on 5 May 2020).
[12] Gratzer, D. et al. (2020), Our Digital Moment: Innovations and Opportunities in Digital Mental Health Care, SAGE Publications Inc., http://dx.doi.org/10.1177/0706743720937833.
[21] Ipsos (2020), The COVID-19 Pandemic’s Impact on Workers’ Lives: 28-country Ipsos survey for The World Economic Forum, https://www.ipsos.com/sites/default/files/ct/news/documents/2020-12/impact-of-the-covid-19-pandemic-on-workers-lives-report.pdf (accessed on 19 February 2021).
[25] Kamerāde, D. et al. (2019), “A shorter working week for everyone: How much paid work is needed for mental health and well-being?”, Social Science and Medicine, Vol. 241, p. 112353, http://dx.doi.org/10.1016/j.socscimed.2019.06.006.
[17] Mental Health America (2020), The State of Mental Health in America, Mental Health America, https://mhanational.org/issues/state-mental-health-america (accessed on 11 February 2021).
[7] NatCen Social Research (2021), Society Watch 2021: Mental health report, NatCen Social Research, https://www.natcen.ac.uk/media/2050456/Society-Watch-2021-Mental-Health-Should-We-Be-Worried.pdf (accessed on 3 May 2021).
[16] National Council for Behavioral Health (2020), Demand for Mental Health and Addiction Services Increasing as COVID-19 Pandemic Continues to Threaten Availability of Treatment Options, https://www.thenationalcouncil.org/press-releases/demand-for-mental-health-and-addiction-services-increasing-as-covid-19-pandemic-continues-to-threaten-availability-of-treatment-options/ (accessed on 11 February 2021).
[19] Oakman, J. et al. (2020), “A rapid review of mental and physical health effects of working at home: how do we optimise health?”, BMC Public Health, Vol. 20/1, p. 1825, http://dx.doi.org/10.1186/s12889-020-09875-z.
[27] OECD (2021), OECD Economic Outlook, Interim Report March 2021, OECD Publishing, Paris, https://dx.doi.org/10.1787/34bfd999-en.
[3] OECD (2021), “Supporting young people’s mental health through the COVID-19 crisis”, OECD Policy Responses to Coronavirus (COVID-19), OECD Publishing, Paris, https://doi.org/10.1787/84e143e5-en.
[26] OECD (2020), Job retention schemes during the COVID-19 lockdown and beyond, OECD Publishing, Paris, https://doi.org/10.1787/0853ba1d-en.
[5] OECD (2015), Fit Mind, Fit Job: From Evidence to Practice in Mental Health and Work, Mental Health and Work, OECD Publishing, Paris, https://dx.doi.org/10.1787/9789264228283-en.
[2] OECD (2012), Sick on the Job?: Myths and Realities about Mental Health and Work, Mental Health and Work, OECD Publishing, Paris, https://doi.org/10.1787/9789264124523-en.
[28] OECD (2011), OECD Employment Outlook 2011, OECD Publishing, Paris, https://dx.doi.org/10.1787/empl_outlook-2011-en.
[23] Persol Research Institute (2020), Daiyonkai shingata koronauirusu taisaku ni yoru terewāku e no eikyō ni kansuru kinkyū chōsa [4th urgent survey on the impact of new coronavirus countermeasures on telework], https://rc.persol-group.co.jp/news/202012160001.html (accessed on 17 February 2021).
[24] PwC (2021), It’s time to reimagine where and how work will get done: PwC’s US Remote Work Survey, https://www.pwc.com/us/en/library/covid-19/us-remote-work-survey.html#content-free-1-0f39 (accessed on 18 February 2021).
[4] Smith, N., I. Taylor and V. Kolbas (2020), Exploring the relationship between economic security, furlough and mental distress, https://www.natcen.ac.uk/our-research/research/exploring-the-relationship-between-economic-security,-furlough-and-mental-distress/.
[13] Torous, J. and M. Keshavan (2020), “COVID-19, mobile health and serious mental illness”, Schizophrenia Research, http://dx.doi.org/10.1016/J.SCHRES.2020.04.013.
[29] van Gool, K. and M. Pearson (2014), “Health, Austerity and Economic Crisis: Assessing the Short-term Impact in OECD countries”, OECD Health Working Papers, No. 76, OECD Publishing, Paris, https://dx.doi.org/10.1787/5jxx71lt1zg6-en.
[9] WHO (2020), The impact of COVID-19 on mental, neurological and substance use services: results of a rapid assessment, World Health Organization, Geneva, https://www.who.int/publications/i/item/978924012455.
[30] WHO (2017), Depression and Other Common Mental Disorders Global Health Estimates, https://www.who.int/mental_health/management/depression/prevalence_global_health_estimates/en/ (accessed on 3 May 2021).
Contact
Stefano SCARPETTA (✉ [email protected])
Francesca COLOMBO (✉ [email protected])
Emily HEWLETT (✉ [email protected])